Endodontics
ROOT CANAL TREATMENT (RCT)
Root canal treatment (also known as endodontic therapy) is a dental procedure used to treat infection or damage to the pulp (the innermost part) of a tooth. The pulp contains nerves, blood vessels, and connective tissue. When this pulp becomes infected due to deep decay, trauma, or repeated dental procedures, it can cause pain and lead to the death of the tooth if left untreated.
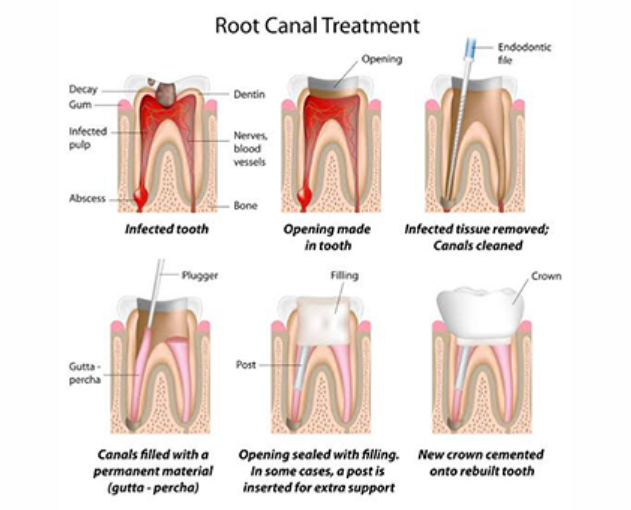
Here’s an overview of what happens during a root canal:
- Diagnosis and Preparation: The dentist or endodontist will take an X-ray to assess the extent of the infection and identify the tooth’s structure. Local anesthesia is administered to numb the area around the tooth.
- Accessing the Pulp: The dentist drills a small hole into the crown (top part) of the tooth to access the pulp chamber and root canals.
- Removing the Infected Pulp: The infected or damaged pulp is carefully removed from the tooth using specialized instruments. This step is important to stop the infection from spreading and to relieve any pain.
- Cleaning and Shaping: Once the pulp is removed, the empty space is cleaned and shaped to prepare it for filling. This also helps remove any remaining bacteria and prevents further infection.
- Filling the Canals: After cleaning, the root canals are filled with a biocompatible material, usually gutta-percha, to seal them and prevent re-infection.
- Sealing the Tooth: In some cases, a temporary filling is placed in the access hole, and a crown is added in a follow-up appointment to provide long-term protection.
- Restoration: After the procedure, the tooth is typically restored with a crown to protect it from breaking and to restore its function.
Why a Root Canal is Needed:
- Tooth Decay: Extensive decay that reaches the pulp.
- Infection: Bacteria entering the pulp through cracks or breaks in the tooth.
- Trauma: Injury or trauma to the tooth, even if there is no visible crack, can damage the pulp.
Symptoms Indicating You Might Need a Root Canal:
- Severe tooth pain, especially when chewing or applying pressure.
- Sensitivity to hot or cold that lasts even after the stimulus is removed.
- Swelling and tenderness in the gums near the affected tooth.
- Darkening of the tooth.
Benefits of Root Canal Treatment:
- Pain Relief: Root canal treatment can provide significant relief from pain caused by infection or inflammation of the pulp.
- Tooth Retention: Instead of extracting the tooth, root canal treatment allows you to save it, maintaining its function and appearance.
- Prevention of Infection: Removing infected tissue prevents the infection from spreading to other teeth or parts of the body.
Here are some frequently asked questions (FAQs) about root canal treatment, along with their answers:
- What is a root canal?
A root canal is a dental procedure used to treat infection or damage inside the pulp (the soft tissue) of a tooth. It involves removing the infected or damaged pulp, cleaning and disinfecting the inside of the tooth, and then filling and sealing it. The goal is to save the tooth and prevent the spread of infection.
- Why do I need a root canal?
You might need a root canal if:
- The tooth pulp is infected or damaged due to deep decay, repeated dental procedures, or trauma.
- You experience severe pain or sensitivity in the tooth.
- There’s swelling or an abscess in the gums.
- There’s a crack or chip in the tooth that has exposed the pulp to bacteria.
- Does a root canal hurt?
Most people believe root canal treatment is very painful, but it is actually quite similar to having a regular filling done. Local anesthesia is used to numb the tooth and surrounding area, so you should not feel pain during the procedure. Afterward, you may experience some mild discomfort or soreness for a few days, but this is usually manageable with over-the-counter pain relievers.
- How long does a root canal procedure take?
The length of the procedure depends on the complexity of the tooth and the extent of the infection. On average, a root canal takes about 1 to 2 hours for a single tooth. Some cases may require more than one visit, especially if there is an infection or if the tooth requires additional work, like a crown.
- What are the symptoms that indicate I need a root canal?
Common symptoms include:
- Severe tooth pain, especially when chewing or touching the tooth.
- Sensitivity to hot or cold that lingers even after the stimulus is removed.
- Swelling or tenderness in the gums near the affected tooth.
- A darkened or discolored tooth.
- A pimple-like bump (abscess) on the gums that may ooze pus.
- Is it possible to avoid a root canal?
Yes, good oral hygiene can help prevent the need for a root canal. Regular brushing, flossing, and dental check-ups help avoid tooth decay and gum disease, which can lead to infection of the pulp. If you catch tooth decay early, your dentist can often treat it with a filling before it progresses to the point where a root canal is necessary.
- How successful is root canal treatment?
Root canal treatment has a high success rate, typically around 90%. Many patients have no issues after the procedure, while others may need follow-up care if the infection returns. A properly restored tooth after a root canal can last for many years or even a lifetime with good care.
- What happens if I don’t get a root canal?
If you don’t treat an infected tooth, the infection can spread, leading to more severe pain, abscess formation, and even the loss of the tooth. In some cases, untreated infection can spread to other parts of the body, leading to more serious health issues.
- What happens after a root canal?
After the procedure, you may experience some mild discomfort or soreness for a few days, which is normal and can be managed with pain relievers. You’ll also need to return for a crown or permanent filling to restore the tooth. The crown helps protect the tooth from fracture and ensures it functions properly.
- Do I need a crown after a root canal?
In most cases, yes, a crown is necessary after a root canal. The procedure often leaves the tooth more fragile because the pulp (which nourishes the tooth) is removed. A crown helps protect the tooth from further damage and restores its strength and appearance.
- How long does it take for the tooth to heal after a root canal?
The tooth itself heals fairly quickly, but it may take a few days for the tissues around the tooth to fully heal. Some mild discomfort is normal, but if pain persists beyond a few days or worsens, it’s important to contact your dentist.
- Can I eat and drink normally after a root canal?
It’s a good idea to avoid chewing on the treated tooth until it is fully restored with a permanent filling or crown. After the procedure, you should wait until the anesthesia has worn off to avoid accidentally biting your cheek or tongue. Stick to soft foods and avoid extreme temperatures in the first few days.
- How much does a root canal cost?
The cost of a root canal can vary based on several factors, such as:
- The location of the tooth (front teeth are typically less expensive than molars).
- The complexity of the procedure (e.g., whether it’s a simple or retreatment).
- Your location, as dental costs can vary by region and country. On average, the cost of a root canal treatment can range from $500 to $1,500 per tooth, with molars often costing more due to their complexity. Additional costs for a crown or other restorations will add to the total cost.
- Is a root canal better than tooth extraction?
Root canal treatment is generally preferred over extraction because it saves the natural tooth. Losing a tooth can lead to more complications, such as shifting of surrounding teeth, bone loss, and the need for more expensive replacements (e.g., dental implants). Root canals allow you to keep your natural tooth while relieving pain and preventing further infection.
- Can a tooth with a root canal still get infected?
Yes, although rare, it is possible for a tooth that has had a root canal to become reinfected. This can happen if the filling or crown doesn’t seal properly, allowing bacteria to re-enter the tooth, or if there were untreated canals during the procedure. If infection occurs, further treatment or retreatment may be required.
- What are the risks of root canal treatment?
Root canal treatment is generally safe, but there are a few risks, such as:
- Reinfection if the tooth isn’t sealed properly.
- Damage to surrounding teeth or tissues.
- Breakage of small tools used during the procedure, though this is rare.
